Patient Education
Hallux Rigidus
|
||||||
Introduction
Physiotherapy in Barrie for Pain Care
Welcome to Skill Builders resource on Hallux Rigidus.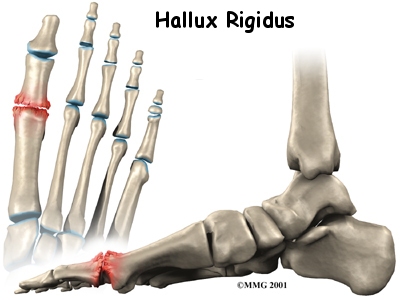 Hallux rigidus is a degenerative type of arthritis that affects the large joint at the base of the big toe (sometimes called the great toe). Degenerative arthritis results from wear and tear on the joint surface over time. The condition may follow an injury to the joint or, in some cases, may arise without a well-defined injury.
Hallux rigidus is a degenerative type of arthritis that affects the large joint at the base of the big toe (sometimes called the great toe). Degenerative arthritis results from wear and tear on the joint surface over time. The condition may follow an injury to the joint or, in some cases, may arise without a well-defined injury.
This guide will help you understand:
- how hallux rigidus develops
- how the condition is diagnosed
- what can be done for the problem
- what Skill Builders approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Foot therapy|limit:15|heading:Hear from some of our *Foot Therapy* patients#
Anatomy
Where does hallux rigidus occur?
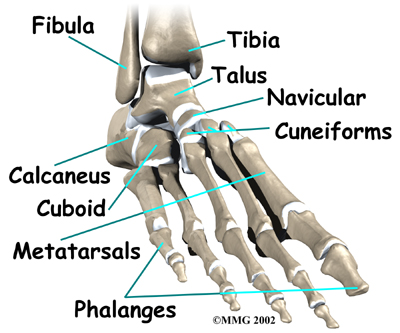
The big toe in medical terms is called the hallux. The joint at the base of the big toe is called the metatarsophalangeal, or MTP, joint. Like any other joint in the body, the joint is covered with articular cartilage, which is a slick, shiny covering on the end of the bone. If this cartilage is injured, it begins a slow process of wearing out, or degeneration. The articular surface can wear away so much that eventually raw bone rubs against raw bone.


Bone spurs form around the joint as part of the degenerative process. The spurs, or bony outgrowths, may restrict the motion in the joint, especially the ability for the toe to bend upward as the body moves forward over the foot, such as when you are taking steps. The big toe becomes very stiff or immobile into this range of motion, hence the reference to rigidity in the name of this condition.
Related Document: Skill Builders Guide to Foot Anatomy
Causes
Why do I have this problem?
Doctors remain uncertain about the true cause of hallux rigidus. A lot of surgeons feel that, in many cases, the condition begins with an injury to the articular cartilage lining the joint, even something as simple as stubbing the big toe. The injury sets in motion a degenerative process that may last for years before symptoms occur that need treatment.
The condition can occur in younger adults but most often affects those who are 50 years or older. Women seem to develop this problem more often than men. There may be a hereditary factor causing this injury since two-thirds of patients have a positive family history of it. Patients who have other family members with hallux rigidus tend to have the problem in both feet (bilaterally).
Other cases of hallux rigidus seem to arise without any type of injury. This suggests that there may be other reasons for the development of the condition. Minor differences in the anatomy of the foot may make it more likely that certain individuals develop hallux rigidus. Anatomical differences could include a slight change in the shape of the end of the bone (e.g., flatter than normal or oddly-shaped), or contracted or tight fascia (connective tissue) under the foot, which increases pressure on the MTP joint. These minor abnormalities may increase the stress that is placed on the joint when you walk. Over many years, this increased stress may add up to degenerative arthritis of the joint.
Symptoms
What does hallux rigidus feel like?
The degeneration at the toe joint causes two problems; pain and loss of motion in the MTP joint. Without the ability of the MTP to move enough to allow the foot to roll through a full step, walking can become painful and difficult. Pain is most noticeable during walking just before toe-off. Pain is increased when wearing shoes that have elevated heels. Bone spurs that develop with this condition can also put pressure on nearby nerves, causing numbness along the inside edge of the big toe.
Diagnosis
How do health care professionals identify the problem?
Diagnosis begins with a complete history of your injury. Your physiotherapist at Skill Builders will ask questions about where precisely the pain is, when the pain began, whether the pain gradually developed over time or if there was a specific injury that started the pain, and what movements aggravate or ease the pain. They will also ask if there is any swelling or weakness noticed in the foot or toe.
Next your physiotherapist will do a physical examination. Your physiotherapist will palpate all around the foot and toe to determine your most tender point. They will also look for swelling or redness in the area. Next they will check the strength of your muscles in your foot and calf. They will ask you to resist certain movements while checking for pain as well as strength deficits, and will ask you to relax as they assess how much general movement is in the toe joint as well as the other joints of the foot and the ankle.
Your therapist will want to observe how you naturally stand, how you walk, and may ask you to do specific movements such as squat on one foot, jump, or jog. They may also want to look at your shoes for their natural wear and tear, which can provide needed information on how you use your foot everyday while you walk.
Diagnosis of hallux rigidus is usually apparent after a physical examination, but X-rays may still required to appreciate the extent of the degeneration and presence of bone spur formation. X-rays also show the shape of the metatarsal head, amount of joint space, and presence of cartilage loss. This information can help direct treatment. MRIs or CT scans are only needed when the X-rays come back normal but some type of lesion is suspected.
Skill Builders provides services for physiotherapy in Barrie.
Treatment
What can be done for the condition?
Nonsurgical Medical Treatment
Treatment begins with anti-inflammatory medications to control the pain, swelling, heat, and redness of the degenerative arthritis. Anti-inflammatory medications may take as long as 7-10 days to become effective. Physiotherapy treatment at Skill Builders can also help the symptoms of hallux rigidus.

If oral anti-inflammatory medications do not help then an injection of cortisone into the joint may give temporary relief of symptoms. A cortisone shot usually works within 24 hours. As with any injection into a joint, a small risk of infection exists with this procedure.
Nonsurgical Rehabilitation
The initial goal of treatment at Skill Builders will be to decrease the discomfort in your foot. Your physiotherapist may use electrical modalities such as ultrasound or interferential current to reduce your pain. Moist heat or ice may also be recommended as a pain-reliever. Often patients prefer heat to ice when dealing with this condition, but both can be effective. A hands-on treatment such as soft-tissue massage to the muscles of the foot and calf as well as traction and mobilizations of the big toe joint and other joints of the ankle or foot may be done to assist both your pain as well as to gently stretch the tissues and encourage the joints to move within their normal range of motion.
In addition to assisting with the pain and swelling, your physiotherapist will prescribe some simple stretching and strengthening exercises for the foot and toe to combat the progression of the injury. The stretching exercises will focus on lengthening the tissues on the sole of the foot as well as those of the calf in order to improve the extension (bending upwards) ability of the big toe. Walking, provided it is not too painful to do and can be done with proper alignment, also assists with improving the toe range of motion. Walking uphill is particularly helpful for the big toe joint range of motion but for many patients this is too painful and cannot be done for a while until the joint pain settles. It should be noted, however, that most exercises, which aim to improve the range of motion of the toe, will likely cause some pain as you push towards the end range of available motion. This discomfort is both normal and also expected as the idea is to improve the existing extension range of motion. The pain caused by toe extension range of motion exercises, however, should not be more than a mild discomfort, and should ease not long after you finish your exercises or therapy session. If your pain is greater than this, lasts for hours, or causes you to limp then you are going too hard with your exercises and you should ease the intensity of your stretches.
Exercises to strengthen the muscles that lift your arch may also be prescribed. All exercises prescribed for hallux rigidus aim to encourage proper foot, and lower limb alignment and biomechanics such that unnecessary forces are minimized through the great toe, particularly with ambulation. Helping your foot to maintain this alignment through your daily activities is crucial. The term joint proprioception describes your joint’s ability to know where it is in space without you having to consciously think about it. Adequate proprioception is required to maintain good foot alignment when walking or running, particularly on unsteady or uneven surfaces.
Your therapist may also prescribe exercises that target the muscles of your hips and knees as well as your core area. The hip joint is the main controller of the knee and foot position, therefore weakness in this area can significantly affect your lower limb alignment and subsequently alter the forces that are transmitted through your big toe. Core stability weakness can do the same. Proper technique with all exercises is crucial in order to avoid extraneous stress through an already painful toe.
Unfortunately if your condition is advanced then there may be minimal gains in range of motion of the big toe even with regular treatment. In these cases, or in those where pain is unbearable, special shoes with rocker type soles may help relieve some of the pain. A rocker type sole is rounded so you roll over the round portion during your step rather than bending through the painful big toe joint. The shoe, rather than the big toe, takes some of the bending force. This type of shoe may be combined with a metal brace in the sole of the shoe to limit the flexibility of the sole and reduce the overall motion required in the MTP joint. Alterations to your shoe wear may take several weeks to have an effect. Being that the toe will now be getting less bending exercise during walking while using the rocker shoe, your stretching exercises are even more crucial to stop advancement of the joint degeneration and to maintain range of motion in the joint.
As an alternative to a rocker shoe, or sometimes in addition to one, taping the big toe may help in the initial stages of discomfort to relieve some of your pain. Your therapist can tape your toe for you as well as teach you how to do it on your own. Your therapist may also use tape along your arch if they feel it is contributing to poor mechanics in your foot. Unfortunately for advanced hallux rigidus, taping may not be of any use.
The above changes to your footwear and use of tape may allow you to walk with less pain but it is still wise to cut back on more vigorous activities for several weeks during the initial period of treatment in order to allow the inflammation and pain to subside. Your physiotherapist can advise you on alternative activities that allow you to maintain your cardiovascular fitness while you allow the pain in your toe to settle. A stationary cycle, rowing machine, water running or water aerobics are all good alternatives to more stressful activities such as running or walking. Keeping up with a weight program is usually possible if you keep all activities to a stationary standing position or a sitting position, and if excessive loads are limited.
Although the physiotherapy treatment we offer at Skill Builders often provides significant relief from hallux rigidus, if you continue to experience considerable pain or the problem seems to be getting worse, a surgical consult may be required.
Surgery
Surgery may be suggested if all else fails. Several types of procedures are useful in treating this condition.
Cheilectomy
In some cases bone spurs that form on the top of the joint can bump together when the big toe bends upward, or extends. This causes a problem when walking because the big toe needs to bend upward when the foot is behind the body, in order to take the next step. The constant irritation when the bone spurs bump together leads to pain and difficulty walking.
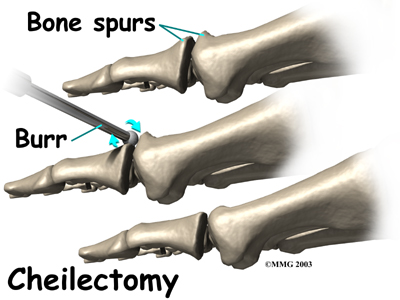
A cheilectomy is a procedure to remove the bone spurs at the top of the joint so that they don't bump together when the toe extends. This allows the toe to bend better and reduces the amount of pain while walking. To perform a cheilectomy, an incision is made along the top of the joint. The bone spurs that are blocking the joint from extending are identified and removed from both the bones that make up the joint. A little extra bone may be taken off to ensure that nothing rubs when the hallux is raised. The skin is closed and allowed to heal.
Joint Fusion
Many surgeons prefer arthrodesis, or fusion, of the MTP joint to relieve the pain. To fuse a joint means to encourage the two bones that form a joint to grow together and become one bone. To perform a fusion, an incision is made into the MTP joint. The joint surfaces are removed. The two surfaces are then fixed with either a metal pin or screw, with the toe turned slightly upward to allow for walking. The bones are then allowed to fuse. The fusion usually takes about three months to become solid.This results in a joint that no longer moves. Wearing a rocker-soled shoe is usually necessary following a fusion to improve your gait.

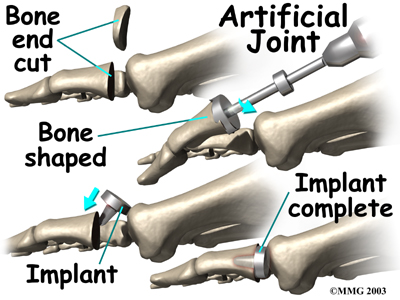
Artificial Joint Replacement
Some surgeons prefer replacing the joint with an artificial joint, similar to what is done in the knee or hip, only much smaller. Replacing the joint with an artificial joint is usually recommended for moderately involved joints. (Many surgeons, however, believe that arthrodesis or fusion still produces better results for patients with severe hallux rigidus.)
In this procedure, one of the joint surfaces is removed and replaced with a plastic or metal surface. This procedure may relieve the pain and preserve the joint motion. The major drawback to this procedure is that the artificial joint will probably not last a lifetime and will require more operations later if it begins to fail.
To perform an artificial joint replacement, an incision is first made on the top of the big toe over the MTP joint. Once the joint is surgically entered, the arthritic joint surface of the proximal phalanx (the first bone of the big toe) is removed. The hollow marrow area of the proximal phalanx is prepared with special instruments so that the artificial joint surface will fit snugly into the bone. Different sized implants are tried, and the toe is moved through a range of motion to help determine if the fit is proper.
Once the surgeon is satisfied that everything fits, the artificial joint surface is implanted. The joint capsule and skin incision are then closed with small stitches.
There are actually several different ways to accomplish a joint replacement for hallux rigidus. A total joint replacement removes and replaces both sides of the joint. This type of procedure requires a conical stem that sits down inside the toe bones on either side of the joint. The implants can be made of ceramic, titanium, cobalt-chrome, or titanium combined with polyethylene (plastic) parts.
Metatarsal hemiarthroplasty replaces just one side of the joint; the one between the bone closest to the middle part of the foot (metatarsal) and the middle phalangeal bone. Limited studies have been done using this approach but patient satisfaction is reportedly high with few implant failures or need for revision surgery.
Other Procedures
There are other surgical procedures that are slight variations of these three approaches. For example, cheilectomy may be combined with a phalangeal osteotomy. With the osteotomy the surgeon removes a wedge-shaped piece of bone from the middle toe bone in order to take pressure off the joint. Some patients can be successfully treated with just the osteotomy procedure.
Another alternative approach (more for the younger patient) is the interpositional arthroplasty. In this procedure, the surgeon removes the base of the toe bone (phalange) and places a "spacer" in the hole left. The spacer is made up of a rolled up piece of tendon. The surgeon may have to release the tendon that inserts into the base of the phalange for this to work best. This decision is made at the time of the surgery.
After Surgery
Your post-surgical treatment will depend on what you have had done with your toe. Generally, however, it will take about eight weeks before the bones and soft tissues are well healed. You may be placed in a wooden-soled shoe or a cast during this period to protect the bones while they heal. You will probably need crutches briefly; a physiotherapist at the hospital will help you learn to use your crutches and ensure that you are safe using them on level ground as well as stairs.
The incision is protected with a bandage or dressing for about one week after surgery. The stitches are generally removed in 10 to 14 days. However, if your surgeon used sutures that dissolve, you won't need to have the stitches taken out.
During your follow-up visits, X-rays will probably be taken so that the surgeon can follow the healing of the bones if a fusion was performed. X-rays are also important if an artificial joint was used to make sure the implant is properly aligned and positioned.
Post-Surgical Rehabilitation
Physiotherapy at Skill Builders can begin as soon as your surgeon advises it. Again, the timing of rehabilitation depends on exactly what has been done in your individual case.
Once you being physiotherapy at Skill Builders our initial goal will be to decrease any pain you have from the surgical procedure itself. Depending on what surgery you have had your therapist may use modalities such as interferential current, ultrasound, ice, or moist heat to reduce the pain. Gentle massage and light mobilizations or traction to the joints of the toe and foot can also assist with pain and any ongoing swelling in addition to improving mobility of the joints. If your joint has been fused, then mobilizations of the fused joint, of course, are of no use, but other joints around the area may require this treatment.
Both the range of motion and strength in your foot (and likely your entire low limb) will be decreased due to the surgical procedure that has been done as well as your altered gait pattern post surgery. Your physiotherapist will prescribe stretching exercises for your toe, foot and calf, as well as strengthening exercises for the same areas. Strengthening exercises may be as simple as picking up marbles with your toes or may include the use of exercise tubing or small elastics. Since the alignment of the foot is maintained by not only the muscles of the foot, but also those of the hip, knee, and core area, we will also prescribe strengthening exercises for these areas. Maintaining proper alignment is particularly important to avoid further problems with the foot and surgical toe. If exercises are too painful on land your therapist may recommend that you do them in a pool, your home tub, or even a pail of warm water so long as your surgical wound is ready for water immersion.
As you get stronger your therapist will prescribe more difficult exercises such standing on your foot on an uneven surface, repetitively raising up onto your toes, and then raising up onto your toes and maintaining this position to improve muscle endurance. These exercises will improve muscle strength and endurance but also improve your foot’s proprioception, or ability to know where it is in space without you having to look at it. Once your foot is mobile and strong enough, we will encourage you to do a short period of uphill walking which helps to both improve the range of motion in your toe and also increase the strength of the foot and calf.
At Skill Builders we believe that it is important for you to maintain your cardiovascular fitness while you are recovering from the surgery for your toe. Although heavy endurance walking or running will not be recommended until a bit further on in your recovery, in the early stages you can still use a stationary cycle, a rowing machine, or get into the pool once the surgical wound is healed to partake in water running or water aerobics. A weight program for your upper extremities, core area, and other leg may be continued early on in your recovery if you have clearance from your doctor and provided that all exercises are in the seated position and do not put stress through your healing toe.
The final part of our treatment at Skill Builders will be to ensure that you are walking with a proper gait. Being that each person takes thousands of steps per day, if you are walking inefficiently or with poor alignment, it can quickly and easily lead to further pain and problems in your foot or up into your ankle, knee, hip, or even low back. A period on crutches or in a cast or brace often leads in itself to a poor walking pattern that carries on once you are off the crutches or out of the brace or cast. Your physiotherapist will address any abnormal walking pattern and teach you how to correct it. The strengthening exercises that we prescribe, as mentioned above, will be important to gain enough strength and control to walk normally after your surgery.
During your follow-up visits with your surgeon, X-rays are usually taken so that the surgeon can follow the healing of the bones and determine how much correction has been achieved.
Generally rehabilitation after surgery for hallux rigidus goes extremely well. If however, you are not improving as your physiotherapist at Skill Builders would expect, we will ask you to follow up with your surgeon to confirm that there are no complications from the surgery or problems with any hardware you may have implanted in your foot.
Portions of this document copyright MMG, LLC
Skill Builders provides services for physiotherapy in Barrie.


